 Integrated post-cardiac arrest care is now the 5th link in the AHA adult chain of survival. Topics of focus for post-cardiac arrest care include (TTM) Targeted Temperature Management, hemodynamic and ventilation optimization, immediate coronary reperfusion with PCI (percutaneous coronary intervention), glycemic control, neurologic care and other technical interventions. To be successful, post-cardiac arrest care requires an integrated multidisciplinary approach.
Integrated post-cardiac arrest care is now the 5th link in the AHA adult chain of survival. Topics of focus for post-cardiac arrest care include (TTM) Targeted Temperature Management, hemodynamic and ventilation optimization, immediate coronary reperfusion with PCI (percutaneous coronary intervention), glycemic control, neurologic care and other technical interventions. To be successful, post-cardiac arrest care requires an integrated multidisciplinary approach.
For the purposes of this site, the review of post-cardiac arrest care interventions will focus primarily on immediate post-arrest interventions and aspects that you will most likely be tested on.
You are viewing: When Titrating Inspired Oxygen Which Arterial Oxyhemoglobin
For a complete review of the subject refer to your AHA provider manual. (pages: 150-158)
(TTM) Targeted Temperature Management
TTM which was previously called therapeutic hypothermia is the only intervention that has been shown to improve neurological outcomes after cardiac arrest. Induced hypothermia should occur soon after ROSC (return of spontaneous circulation). The decision point for the use of therapeutic hypothermia is whether or not the patient can follow commands. (lack of meaningful response to verbal commands)
One of the most common methods used for inducing therapeutic hypothermia is a rapid infusion of ice-cold (4° C), isotonic, non-glucose-containing fluid to a volume of 30 ml/kg. The optimum temperature for therapeutic hypothermia is 32-36 ° C (89.6 to 96.8 ° F). A single target temperature, within this range, should be selected, achieved, and maintained for at least 24 hours.
During induced TTM, the patient’s core temperature should be monitored with any one of the following: esophageal thermometer, a bladder catheter in the nonanuric patients, or a pulmonary artery catheter if one is already in place.
Read more : When Are Lychee In Season
Axillary and oral temperatures are inadequate for monitoring core temperatures.
Ventilation Optimization
During the post-cardiac arrest phase, inspired oxygen should be titrated to maintain an arterial oxygen saturation of ≥92-98%. The goal is to avoid hypoxia and hyperoxia. This reduces the risk of oxygen toxicity. Excessive ventilation should also be avoided because of the potential for reduced cerebral blood flow related to a decrease in PaCO2 levels. Also, excessive ventilation should be avoided because of the risk of high intrathoracic pressures which can lead to adverse hemodynamic effects during the post-arrest phase.
Quantitative waveform capnography can be used to regulate and titrate ventilation rates during the post-arrest phase. Visit the link for more details about waveform capnography.
Avoid excessive ventilation. Ventilation should start at 10/min and should be titrated according to the target PETCO2 of 35-45 mmHg.
Hemodynamic Optimization
Hypotension, a systolic blood pressure < 90 mmHg should be treated and the administration of fluids and vasoactive medications can be used to optimize the patient’s hemodynamic status. While the optimal blood pressure during the post-cardiac arrest phase is not known, the primary objective is adequate systemic perfusion, and a mean arterial pressure of ≥ 65 mmHg should accomplish this. A systolic blood pressure greater than 90 mmHg and a mean arterial pressure greater than 65 mmHg should be maintained during the post-cardiac arrest phase.
The goal of post-cardiac arrest care should be to return the patient to a level of functioning equivalent to their prearrest condition.
IV infusions for the control of post-arrest hypotension:
- IV Fluid Bolus: Give 1-2 L of normal saline or LR
- Epinephrine 2-10 mcg/min
- Dopamine 5-20 mcg/kg/min
- Norepinephrine 0.1-0.5 mcg/kg/min
Other considerations
Read more : When Will 2023 Staar Scores Be Released
Moderate glycemic control measures should be implemented to maintain glucose levels within a normal range, and since there is an increased risk for hypoglycemia, attention should be focused on prevention. No specific glycemic target range is recommended at this time.
Every effort should be made to provide coronary reperfusion (PCI), and interventions should be directed with this goal in mind. PCI has been shown to be safe and effective in both the alert and comatose patient, and hypothermia does not contraindicate PCI.
Click below to view the Post-Cardiac Arrest Algorithm Diagram. When finished, click again to close the diagram.
Post-Cardiac Arrest diagram
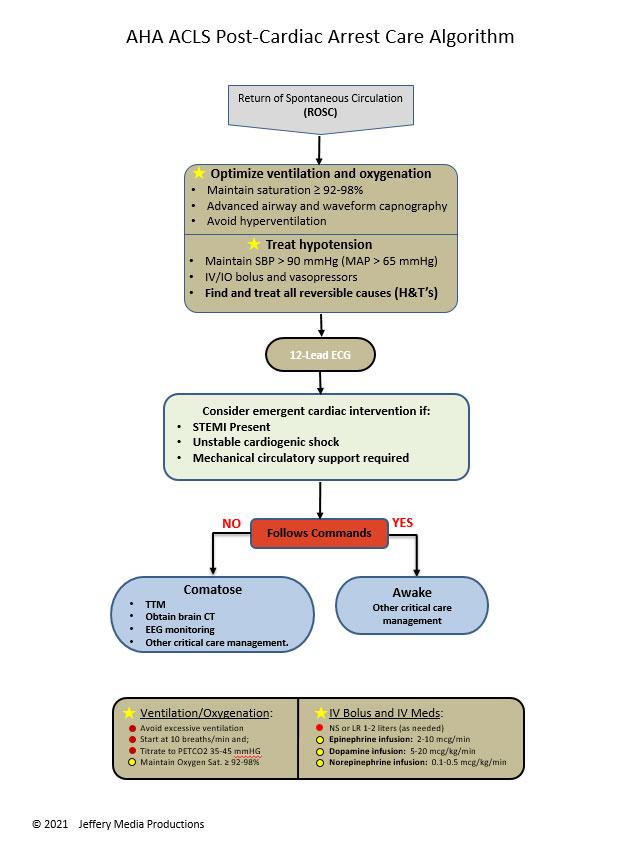
or Download the High Resolution PDF Here. (This will open in another window.)
Source: https://t-tees.com
Category: WHEN
