Ross Hauser, MD
I am going to begin this article with a case history seen at our center and then we will discuss the research that shows a connection between cervical spine instability and neck pain leading to your problems of chronic sinusitis and various other conditions you may suffer from including Eustachian tube dysfunction.
You are viewing: Which Vertebrae Affects Sinuses
As I have stated many times in the articles on our website, people we see rarely suffer from one problem or condition by itself. Tinnitus, vertigo, imbalance, dizziness, and hearing loss are common symptoms of cervical spine instability caused by weak or damaged cervical spine ligaments and are often symptoms of those who are diagnosed with POTS (postural orthostatic hypotension), cardiovascular dizziness, vestibular neuritis, migraines, benign postural positional vertigo, persistent postural perceptual dizziness, or Meniere’s disease, and can have common pathophysiology: Cervicovagopathy. Cervico – a structural problem in the neck that is causing “vago” vagus nerve “pathy” or disease or illness. Cervicovagopathy is then the neck’s altered or broken structure causing compression or disease on the vagus nerve and then on to produce a myriad of symptoms related to dizziness.
Article summary
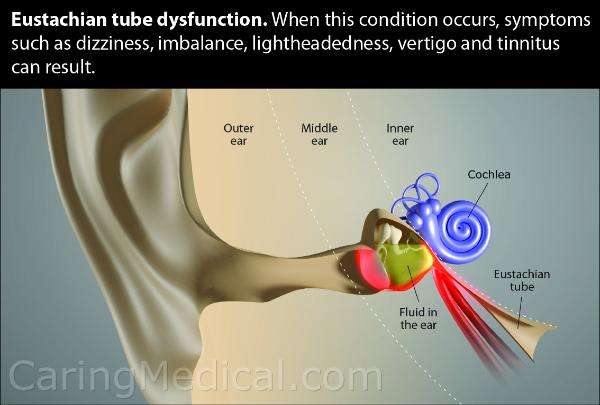
- Eustachian Tube Dysfunction. When this condition occurs, symptoms such as dizziness, imbalance, lightheadedness, vertigo and tinnitus can result.
- A 25-year-old college student with chronic sinusitis and Eustachian tube dysfunction.
- Nothing helped his Eustachian tube dysfunction, worse, over the next six months, the symptoms themselves were getting worse.
- A clue about Eustachian tube dysfunction from a deviated uvula.
- What a deviated uvula can mean in patients with “neurologic-type” symptoms.
- When it comes to strange symptoms, doctors often report cases that “stumped” them. This is where we call in the specialists, the medical research papers.
- Low vagal tone or vagus nerve injury. A connection to the trigeminal nerve will also be made.
- The cervical spine and “cervicogenic otoocular syndrome.”
- A clue suggesting vagus nerve compression is the problem: Some people with a functional disorder of the upper cervical spine have problems related to vision.
- Clicking in the ears, eustachian tube dysfunction, and chronic sinusitis. They are all connected.
The main mechanisms by which cervical instability causes dizziness are:
- Tension on the cervical spinal cord and or brain stem
- Neck Proprioception dysfunction (The movements of your head and neck do not match).
- Vagus nerve injury vagopathy
- Atlas malalignment
- Intracranial hypertension vestibular neuritis blockage of cerebral fluid vertebral carotid artery occlusion dysautonomia internal jugular venous compression vertebral subluxation.
Eustachian Tube Dysfunction. When this condition occurs, symptoms such as dizziness, imbalance, lightheadedness, vertigo and tinnitus can result.
A 25-year-old college student with chronic sinusitis and Eustachian tube dysfunction
A 25-year-old college student became a patient at Caring Medical. He suffered from a myriad of symptoms including chronic sinusitis. As with many 25-year-old men he engaged in sports, some high contact sports. He also worked out, trained, and ran. He also told us about the many high-speed impacts he had with other players during games. He reported a number of hits to the head. As his symptoms progressed his activity levels fell to a now “couch potato,” status.
He is a nose breather
After one particular game where he was involved in a high-impact collision, our patient started to get popping sounds and a sensation of grinding in his neck. After the collision, he felt as if his nose was all plugged up. This presented a problem for him as he stated he was always a nose breather. As this symptom worsened, he stated he would spend 15-30 minutes every morning blowing his nose and using other decongest aids and techniques so he could breathe out of it.
Even when he was successful at this, this would only allow him to breathe out of his nose for a few minutes, then it would get stopped up again. He described it as having a really bad cold or flu all the time. With the stopped-up nose came ear fullness, hearing loss, tinnitus, and dizziness. His ears popped constantly, like balloons. He noticed the symptoms were worse when he looked down at his phone or the ground.
He saw many doctors, including ENTs, allergists, primary care physicians, emergency room physicians, a gastroenterologist, a cardiologist, and neurologists. They all said he had allergies and prescribed different types and variant strength decongestants, steroids, antihistamines, and other drugs to no prevail. He was also prescribed anti-anxiety medications.
- The problem with his Eustachian tube did not seem to be one of primary inflammation being the cause, and as you probably know first hand if you have been treated for Eustachian tube dysfunction, it is all about inflammation. If the Eustachian tube is inflamed it cannot open properly. If it cannot open properly hearing problems, ear fullness, and tinnitus set in. This person had been through many courses of anti-inflammatories and other treatments without resolution of his issues.
Nothing helped his Eustachian tube dysfunction, worse, over the next six months, the symptoms themselves were getting worse.
A clue from a deviated uvula
Why then were his anti-inflammatories not effective? Why were his anti-histamines not effective?
Again, as we typically see, this patient had various conditions and symptoms. Already mentioned above were trips to a gastroenterologist to track down digestive problems, a cardiologist to rule out heart problems, and neurologists to determine if neurological deficits and problems were at play here. As these other possible causes were being ruled out, what could be left? For some people, it is cervical spine instability and compressive problems in the neck. Nerve impingement can be going on.
When this person came into our center, it was after a screening process to determine if cervical spine instability could be realistically thought of as a cause of his problems. Once we suspected cervical spine instability as the underlying cause of his problems, we asked about other cervical instability symptoms including headaches, visual changes, neck/head, and scalp pain, he noted he had all of them. In fact, his neck was causing him a lot of pain and discomfort, enough so that he had sought out chiropractic care. Of which he did say that he did find relief, but only on a temporary basis.
A possible clue: A deviated uvula. What is this?
Upon his initial examination, we noted that he had a deviated uvula sitting to the left of where it should be. This typically signals right side vagus nerve injury and low vagal tone which correlated with his right side tinnitus from Eustachian tube dysfunction being worse than left. His digital motion x-ray showed a loss of the cervical curve (he had a military curve), forward atlas (atlas anterior subluxation), and significant C1-C2 (atlantoaxial) instability.
What does all this mean?
Let’s stop the case history here so we can go deeper into the problems discovered during our examination and have a better understanding of what is happening. We will also have some specialists come in, in the form of research papers that will help you understand what we saw in this patient’s first examination.
Read more : Which Is Better Viking Or Avalon River Cruises
We mentioned:
- A deviated uvula
- Low vagal tone or vagus nerve injury. A connection to the trigeminal will also be made.
- A loss of the natural cervical spine curve.
Now let’s explore what is happening here starting with the deviated uvula.
A deviated uvula: In this video, Dr. Hauser explains what a deviated uvula can mean in patients with “neurologic-type” symptoms.
There are various clues that the vagus nerve is involved in the different and complex neurological, cardiac, and gastrointestinal problems some people have. One of the simplest ways to send us down the path of vagus nerve function is to simply look down the throat of the patient and see if the uvula (the small finger-like tissue that hangs at the back of the soft palate) deviates to one side, we call that a deviated uvula and a deviated uvula is one of the biggest clues that the vagus nerve is not functioning correctly.
We know, you may be saying to yourself, “I had all these tests, my doctors can’t find anything, how can looking down my throat tell me something the tests did not?”
- Many patients we see have, have ear pain, ear fullness, or sensitivity to sound.
- Some of these people have a long medical history that may include visits to the ENT and other specialists and doctors. Some may get a diagnosis of Meniere’s disease.
- In many of these patients, their problems of tinnitus, Meniere’s disease, dizziness, ear fullness, decreased hearing, or sensitivity to sound may be traced to problems of cervical spine/neck instability.
- Cervical spine instability can cause impingement or pressure on the various cranial nerves including the vagus nerve.
- Many times this factor is not even looked for as many doctors are not aware that this could be the problem.
- For many people, their long medical history of unresolved neurological type problems may have their roots in cranial nerve impingement in the cervical spine.
When it comes to strange symptoms, doctors often report cases that “stumped” them. This is where we call in the specialists, the medical research papers.
When it comes to strange symptoms, doctors often report cases that “stumped” them. By reporting these cases it is hoped that this will help those health care providers after they see these cases and maybe figure out something beneficial for future patients who may have similar symptoms.
What we will focus on here is a report of a uvula deviation and how this may be a way to screen unresponsive or difficult to treat or understand neurological and digestive-type symptoms.
Here is a case reported in the Journal of Child Neurology. (1) It is about a 7-year-old boy who displayed symptoms very similar to our patient. Here is that story:
- A 7-year-old boy was seen by doctors because of a sudden change to nasal speech, dysarthria (muscle malfunction when talking) for words with explosive consonants in speech, and nasal regurgitation of fluids.
- The symptoms arose over 1 week following a capricious (sudden and unaccountable) episode of acute asthmatic bronchitis.
- Physical and neurologic examinations were normal except for a left deviation of the uvula, accompanied by a “curtain” movement of the posterior pharyngeal wall against the opposite side, and a left deviation of the protruded tongue.
EXPLANATORY NOTE: Look at what is happening here. The boy had a deviation of the uvula and a “curtain” movement of the posterior pharyngeal wall (the back of the throat). The curtain movement is an involuntary movement of the soft palate at the back of the throat. The muscles of the palate move up and down like a curtain rising and falling. This problem is also associated with clicking in the ears. Clicking in the ears is a symptom of Eustachian tube dysfunction.
- No vascular, traumatic, infectious, neoplastic, or neurologic causes could be identified. No therapy was administered. Full recovery occurred 4 months later. The diagnosis was idiopathic (we do not know why he had it or why it went away on its own) vagal and right hypoglossal nerve palsy (Bell’s palsy).
So what these doctors pointed out was there was a case of asthmatic bronchitis, which turned into other symptoms, it affected the vagus and hypoglossal nerves.
This case is presented to show the interplay between an infection, in this case, asthmatic bronchitis and vagus nerve malfunction. How one can affect the other.
Low vagal tone or vagus nerve injury. A connection to the trigeminal nerve will also be made.
An important aspect of vagus nerve function is its role in the regulation of middle ear pressure by opening the auditory tube or Eustachian tube. The Eustachian tube connects the middle ear cavity with the nasopharynx. Normal opening of the Eustachian tube equalizes atmospheric pressure in the middle ear and clears mucus from the middle ear into the nasopharynx. The Eustachian tube needs to be open during normal swallowing, as just that noise could damage the sensitive nerve endings and structures in the inner ear. The vagus nerve innervates the levator veli palatini one of the key muscles that open the Eustachian tube. The other muscle that opens the Eustachian tube is the tensor veli palatine innervated by the trigeminal nerve. If the Eustachian tube on one side of the head were unable to open and close properly then secretions would build up in the middle ear, causing a pressure gradient between the middle ear, atmosphere, and the other middle ear cavity. When the pressure inside one middle ear cavity is different than the other side it can cause many symptoms including dizziness, hearing loss, ear discomfort, ear fullness, pressure in the ears (as if submerged in water), as well as pain in the ears.
The cervical spine and “cervicogenic otoocular syndrome.”
Next, we are going to visit the opinion of a paper presented in The International Tinnitus Journal. (2) Here the researchers sought to make a connection between cervical spine disorders and hearing problems that would eventually result in tinnitus and Ménière’s disease. Here are the summary learning points:
- The researchers observed 420 patients who had fullness in the ear, episodic vertigo, fluctuating hearing, and tinnitus over a four-year period.
- They noted 182 patients showed normal hearing levels, a mild Eustachian tube dysfunction, normal SP/AP ratios (summating potential/action potential as a means to measure hearing disorders), mydriasis (pupil dilation) on the side of the affected ear, and a functional disorder of the upper cervical spine.
- These patients responded to conservative management, particularly physiotherapy.
- Additionally, 51 patients showed normal hearing levels, a mild Eustachian tube dysfunction, an elevated SP/AP ratio suggesting endolymphatic hydrops, mydriasis on the side of the affected ear, and a functional disorder of the upper cervical spine.
- Note: Endolymphatic hydrops is a disorder of the middle ear caused by vestibular system dysfunction.
- The vestibular system is the body’s sensory system that regulates balance and spatial orientation (the understanding of where you are in your environment).
- It sits in the inner ear and works by adjusting fluid levels that act as the balance mechanism.
- We set our awareness of our place in space by using the ground as the constant place of orientation. We can keep our balance when we walk because we understand the ground is the constant and our vestibular system makes constant involuntary adjustments to “keep things steady,” to prevent motion from creating dizziness or sway.
- Note: Endolymphatic hydrops is a disorder of the middle ear caused by vestibular system dysfunction.
- The patients of the study were given a diagnosis of cervicogenic otoocular syndrome.
- Within this group, 43 patients did not respond to preceding conservative management, and 3 patients developed Ménière’s disease within 12 months.
- Also within this group, 8 patients responded to physiotherapy only, with a return of the SP/AP ratio to normal levels.
- A total of 187 patients had a sensorineural hearing loss, an elevated SP/AP ratio, mydriasis on the side of the affected ear, a functional disorder of the upper cervical spine.
- Of the patients, 186 had mild Eustachian tube dysfunction and had been diagnosed with Ménière’s disease.
- Patients with COO syndrome invariably responded to the insertion of a middle-ear ventilation tube, with the return of the SP/AP ratio to normal levels and relief of symptoms. Patients with Ménière’s disease had a mixed response. The cervicogenic otoocular syndrome is suspected to be a forerunner of Ménière’s disease.
What is being suggested here? Simply that a functional disorder of the upper cervical spine can cause hearing problems.
A brief discussion of Meniere’s disease
I want to briefly touch on Meniere’s disease here. For more extensive research on this problem, please see my articles: Meniere’s Disease and Fluid build up in the ears – Chronic cerebrospinal venous insufficiency and Ear pain, ear fullness, sound sensitivity, tinnitus, Meniere’s Disease and hearing problems caused by neck instability.
Meniere’s disease is a disorder of the inner ear that causes spontaneous episodes of vertigo – a sensation of a spinning motion – along with fluctuating hearing loss, ringing in the ear (tinnitus), and sometimes a feeling of fullness or pressure in the ear. In many patients, low-frequency hearing loss is seen. Meniere’s disease comprises symptoms related to the Eustachian tube, the upper cervical spine, the temporomandibular joints, and the autonomic nervous system. The cervical spine, temporomandibular joint, and Eustachian tube all are connected through the autonomic nervous system as well as peripheral nerves such as the trigeminal nerve. All of these symptoms can easily appear if some condition were causing fluid to accumulate in the inner ear because of Eustachian tube dysfunction.
A clue suggesting vagus nerve compression is the problem: Some people with a functional disorder of the upper cervical spine have problems related to vision
The people in the above study noted a problem of mydriasis (pupil dilation) on the side of the affected ear.
When the Vagus nerve is injured by compression caused by instability at C1-C2, this can cause vasospasms (narrowing of the arteries and reduction of blood flow). If these vasospasms impact the ophthalmic artery, the artery that supplies blood to the eye and eye area including the orbit – this can lead to some of the symptoms are patients describe to us such as darkening, black spots, or grayness in the vision of one eye.
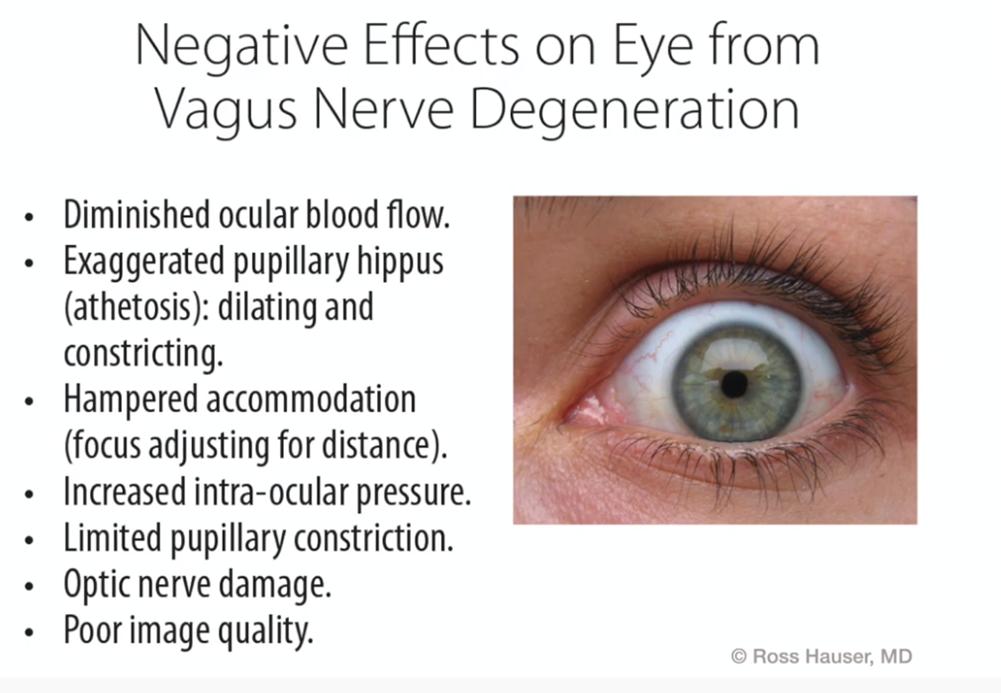
In this image, vision problems caused by cervical spine instability are connected to Diminished ocular blood flow, Exaggerated pupillary hippus dilating, hampered accommodation or human ocular accommodation mechanism or accommodation reflex, Increased intraocular pressure, or elevated intraocular pressure, Limited pupillary constriction, Optic nerve damage.
Clicking in the ears, eustachian tube dysfunction, and chronic sinusitis. They are all connected.
There can be many reasons you have clicking in your ears, there can be many reasons you have chronic sinusitis. There can be many reasons you have both. This article presents one possible answer to why you may have not responded to treatment. That answer is a connection to cervical spine instability and neck pain.
In your research of chronic sinusitis and eustachian tube dysfunction symptoms, you learned that eustachian tube dysfunction is when the eustachian tube that connects the throat to the ears gets clogged. When this happens you can have ear fullness, ear pain, and hearing difficulties associated with a clogged eustachian tube. You learned that this is more frequent in people with sinusitis, allergies, who smoke, and people who are obese.
- Eustachian Tube Dysfunction
- The eustachian tube is the canal that connects the inner ear and the upper throat. It regulates the pressure within the inner ear.
- Eustachian Tube Dysfunction can occur when the muscles of the eustachian tube, the tensor veli palatini, the levator veli palatini, the salpingopharyngeus, and the tensor tympani, do not perform their job of opening and closing the tube. This can cause fluid build-up in one ear as opposed to the other. This can cause problems of inner ear fullness, ear pain, and loss of sense of balance. Cervical spine instability can cause muscle disruption.
What are we seeing in this image?
Proper Eustachian Tube function vs. dysfunction. In this illustration, the proper opening of the Eustachian Tube is shown to require the action of the tensor veli palatini and the levator veli palatini muscles innervated by the vagus and trigeminal nerves. When these muscles do not operate normally, fluid builds up in the middle ear potentially causing the problems of ear discomfort, ear fullness, pressure, pain, dizziness, and even partial or complete hearing loss.
Above I suggested the connection between cervical spinal instability and a patient’s Eustachian tube dysfunction and sinusitis. The surgical research above confirms this connection. Let’s look at the sinusitis part of his problem and also connect that to cervical spine instability.
First, let’s look at a case study in the Journal of Manual and Manipulative Therapy. (3) It looks at possible sinus headaches and the development of rhinosinusitis and a connection to neck pain.
Here are the summary learning points:
- Headaches can be associated with rhinosinusitis and may present a diagnostic challenge because of symptomatic overlap with other recurring headaches.
- Neck pain has received extensive attention in migraine, tension-type, and cervicogenic headaches but not as a comorbid feature of headache in those with rhinosinusitis.
- This study investigated the occurrence of neck pain and cervical musculoskeletal dysfunction in individuals with self-reported sinus headaches.
- Patients in this study (who had an average duration of symptoms of 8.5 YEARS) were asked to assess their Cervical range of motion (ROM), had a cervical segmental examination, muscle endurance, and pressure-pain threshold tests.
- Findings or tests and examinations: “Neck pain and cervical musculoskeletal dysfunction are common among persons with sinus headaches and may be a comorbid feature or contributing factor to headaches attributed to rhinosinusitis. Further research is needed to understand these associations.”
In the research of your symptoms, you have probably uncovered various connections between your neck pain and your problems with a chronic sinus infection, sinusitis, and rhinosinusitis. Here you learned that much like problems with Eustachian tube dysfunction, an inability of the Eustachian tube to drain, you may have a problem with sinus drainage.
Malalignment of C1-C2 can impact sinus drainage
We have many articles and research studies that point out the possible problems misalignment of the C1-C2 or Atlantoaxial instability can cause. As I have also pointed out, the clue to a patient’s problems may lie in the fact that they suffer from many symptoms simultaneously and not from one or two isolated symptoms.
In the story of the patient that we are covering in this article, we see that he had many symptoms. People we see with Atlantoaxial instability can also suffer from drainage problems of the sinus and associated nasal congestion, headaches, hearing problems and ear infections, vision problems, balance, vertigo, dizziness, and nausea among many symptoms. Often they suffer all at once.
When the cervical spine is involved in chronic ear or sinus infections, we suspect that the patient is having a drainage problem. The ear and sinus are not draining. One reason that they are not draining can be a bulging or herniated disc impinging on the cervical nerves in the C1-C2 region.
The start of the chase for the root cause of the problem. The connection between the vagus nerve and the trigeminal nerve and sinus drainage
The vagus nerve, as illustrated below, travels through the cervical spine. It travels especially close to the C1, C2, C3 vertebrae. Cervical spine instability in these regions can cause herniation or pinching of the vagus nerve, which can lead to a disruption of normal nerve communication between the vagus nerve and the trigeminal nerve and trigeminal ganglion. This disruption or herniation of the nerve can cause among the many symptoms of cluster headaches.
What are we seeing in this image?
The vagus nerve, as illustrated here, travels through the cervical spine. It travels especially close to the C1, C2, C3 vertebrae. Cervical spine instability in these regions can cause herniation or pinching of the vagus nerve, which can lead to a disruption of normal nerve communication between the vagus nerve and the trigeminal nerve and trigeminal ganglia. This disruption or herniation of the nerve can cause among the many symptoms of cluster headaches.
In the context of this article, we will simply explore how cervical spine instability impacts the trigeminal nerve and how this impact can prevent your sinus from draining. A more complex understanding of the trigeminal nerve is found here: The evidence for Trigeminal Neuralgia non-surgical treatments.
References
1 Zannolli R, Acquaviva A, D’Ambrosio A, Pucci L, Balestri P, Morgese G. Vagal and hypoglossal Bell’s palsy. Journal of child neurology. 2000 Feb;15(2):130-2. [Google Scholar] 2 Franz B, Altidis P, Altidis B, Collis-Brown G. The cervicogenic otoocular syndrome: a suspected forerunner of Ménière’s disease. International Tinnitus Journal. 1999;5(2):125-30. [Google Scholar] 3 Petersen SM, Jull GA, Learman KE. Self-reported sinus headaches are associated with neck pain and cervical musculoskeletal dysfunction: a preliminary observational case control study. Journal of Manual & Manipulative Therapy. 2019 Aug 8;27(4):245-52. [Google Scholar] 4 Steilen D, Hauser R, Woldin B, Sawyer S. Chronic neck pain: making the connection between capsular ligament laxity and cervical instability. The open orthopaedics journal. 2014;8:326. [Google Scholar] 5 Lee IH, Kim DH, Kim SW, Kim SW. Changes in symptoms of Eustachian tube dysfunction after nasal surgery. European Archives of Oto-Rhino-Laryngology. 2022 Mar 29:1-7. [Google Scholar] 6 Chen T, Shih MC, Edwards TS, Nguyen SA, Meyer TA, Soler ZM, Schlosser RJ. Eustachian tube dysfunction (ETD) in chronic rhinosinusitis with comparison to primary ETD: A systematic review and meta‐analysis. InInternational Forum of Allergy & Rhinology 2022 Jul (Vol. 12, No. 7, pp. 942-951). [Google Scholar] 7 Chen WC, Yang KL, Lin WC, Fang KC, Wu CN, Luo SD. Clinical outcomes of Eustachian tube dysfunction in chronic rhinosinusitis following endoscopic sinus surgery. Journal of the Chinese Medical Association. 2022 Jul 1;85(7):782-7. [Google Scholar]
6259
Source: https://t-tees.com
Category: WHICH
