In 2020, approximately 18% of CMS in network claims were denied. Denials by some plans were as high as 80% and continue to increase.
What is denial management in healthcare medical billing?
Denial management in healthcare is a strategic process that aims to identify and resolve problems leading to medical claim denials.
You are viewing: Which Department Is Responsible For Reviewing And Addressing Claim Denials
 Proactive steps to reduce claim denials include:
Proactive steps to reduce claim denials include:
- Code diagnosis to the highest level of specificity
- Ensure insurance coverage and eligibility
- File claims on time
- Stay current with payor requirements
- Track the claim throughout the entire process
By following these steps, you can effectively mitigate the risk of future denials, ensuring a faster reimbursement and a healthy cash flow.
Why medical billing denials and solutions matter so much
According to AHIMA, denial rates have increased more than 20 percent over the past five years. That is why understanding and managing medical denials is so critical to hospital cash flow.
Denial rates have increased more than 20 percent over the past five years. ~ Source: AHIMA
Case Study: Reduced DNFB by 56%
For example, JTS was engaged with a client whose discharged, not final billed (DNFB) was over $6M and while the facility knew the DNFB was high, they did not know how to address the issue. DNFB is when bills are incomplete due to coding or documentation therefore cannot generate a claim and can be denied due to timely filing.
How did we decrease DNFB?
- JTS unitized nCREAS™ to break down the DNFB by category and created a strategy that worked for them.
- JTS worked with them to identify aged accounts within the DNFB to clear them quickly so timely filing would not be an issue.
- JTS then broke the DNFB down by location and pinpointed which physicians were holding up accounts because of the delay in notes.
- Updated policies and procedures were created for the physicians to improve their processes.
- Result: In a three- month span, JTS reduced the facilities DNFB by 56%.
Understanding the trends and opportunities for improvement in denial management over time and utilizing analytics to provide deep insight leads to a reduction in denials and an increase in profitability.
Types of claim denials
Medical denials can be classified in two categories: soft and hard. Soft denials are temporary and have the potential to be paid but may require a corrected claim to be submitted. Hard denials do not have the potential of being paid and must be written off by the hospital. Human error is the cause of many soft denials. That is why making sure all information is complete and correct is so important.
What are claim rejections vs. claim denials?
While claim rejections and claim denials sound similar, they are very different. Claim rejections are claims that have one or more errors that are identified before the claim is accepted for processing. Certain data requirements were not met, so the claim was returned to the healthcare provider by the payor for corrections before being accepted into the payor system. Reasons for rejections may include incomplete information, biller error or incorrect procedure or ICD code or modifier.
Denied claims have been accepted by the payor, processed and determined to be unpayable. Reasons for denials may include errors or not adhering to the payor contract. The reason for denial must be determined and an appeal or corrected claim made to reconsider the claim.
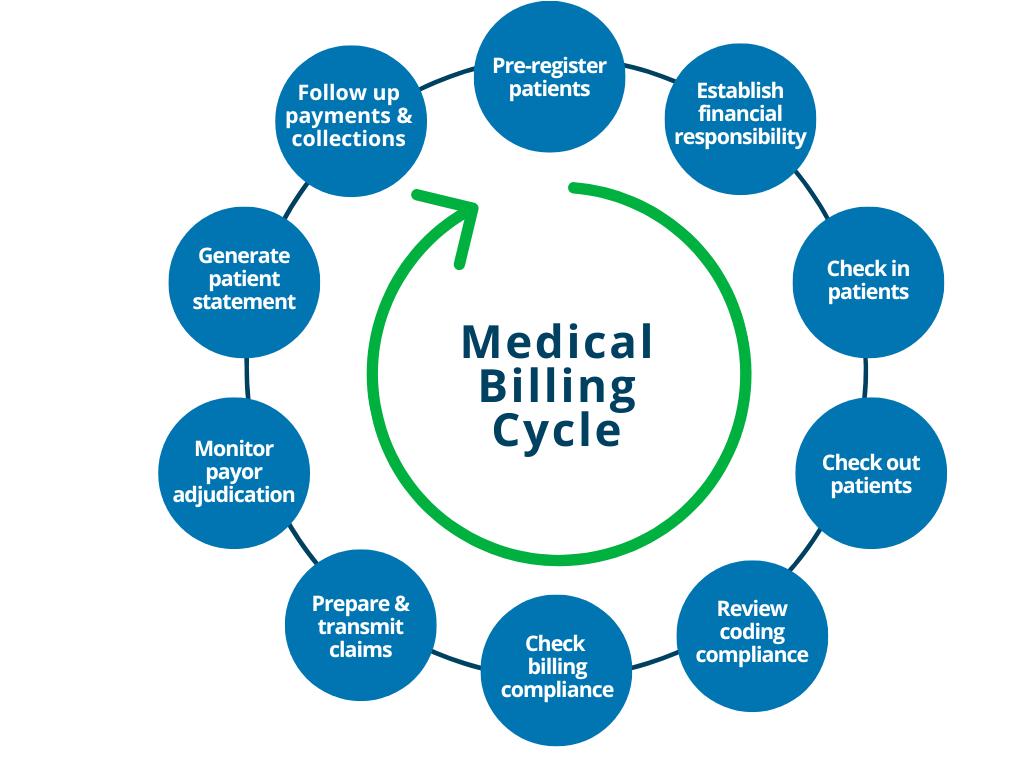
What is the denial management process? How does it work?
The denial management process in medical billing will vary depending on the type and reason for the denial. In general, the claim will need to be reviewed to determine the cause of denial. The payor contract will need to be reviewed to ensure the proper adherence to the guidelines were followed. Supporting documentation or the lack of documentation will need to be determined and reviewed. The claim may be submitted for reconsideration, appeal or follow up will continue until resolution of the claim. For example, for a CO-50 Not Medically Necessary denial, the steps would include the graph below:

Step 1: Identify
What is the first step in denial management?
Denials can be easily identified from resolved accounts. If there is a balance on an account after a response is received from the payor, the claim could be denied or underpaid. The reason for denial or underpayment can very. However, the reason can be found easily after the review of insurance explanation of benefits (EOB). Upon review of the insurance EOB, you can determine which line has been denied or underpaid. After identification of the line item, check the reason/remark codes for the cause for denial. The reason for the denial could be a lack of prior authorization, missing information or issues with coverage. Be sure to track denials and underpayments to assist in future prevention.
What are the top 5 medical billing denials?
Medical billing denials can occur for various reasons. The most common causes for denials include:
- Missing / Lacking information – incomplete, invalid or missing fields on a claim can lead to a denial
- Service Not Covered by Payor – review claim to ensure the service is covered in the payor contract
- Duplicate Claim or Service – claims that have been submitted multiple times without indication of correction will be denied or if the claim was already adjudicated the claim would deny as duplicate
- Limit For Filing Has Expired – timeliness in submitting claims is vital to mitigating the denial management process
- Not Medically Necessary – Claims that do not have a valid diagnosis to support service on claim
The good news is that these causes are preventable with the proper training and attention to detail.
Step 2: Manage
How to manage denied claims? Lowering your claim denial rates
Lowering claim denial rates is essential to timely and optimized reimbursement. There are several ways to decrease denial rates in medical billing.
Proactive denial management
Tips to reduce claim denials include:
- Code diagnosis to the highest level of specificity
- Ensure insurance coverage and eligibility
- File claims on time
- Stay current with payor requirements
- Track the claim throughout the entire process
By following these steps, medical billers can effectively mitigate the risk of future denials and ensure timely payments.
Speed, don’t delay – Common claim delays
Some of the most common delays in processing claims are due to negligence. With the proper training, these delays can be greatly reduced. Some of the top reasons claims get delayed in processing are:
- Incomplete or incorrect information
- Incorrect codes
- Non-Daily translation of claims
- Late submission of claims
- Lack of coordination among staff
- Failing to comply with individual third-party payor requirements
 Make sure billers and coders are educated on the most current rules and regulations for coding. Instituting claim scrubbing software can identify and fix problem claims automatically. This may save time and ensure greater accuracy. Also ensuring a high clean claim rate over 80% will help with a speedy recovery. High clean claim rates result in minimal follow-up and error correction. With workflow education, payment delays will be no more.
Make sure billers and coders are educated on the most current rules and regulations for coding. Instituting claim scrubbing software can identify and fix problem claims automatically. This may save time and ensure greater accuracy. Also ensuring a high clean claim rate over 80% will help with a speedy recovery. High clean claim rates result in minimal follow-up and error correction. With workflow education, payment delays will be no more.
Creating a standard workflow for denial management
Creating a standard workflow is essential for an effective revenue cycle. These four steps will assist in the effectiveness of your billing office.
- Identify
- Identifying if the claim is denied or rejected
- Investigate the reason for non or partial payment
- Manage
- Enforce denial routing
- Ensure all coding related denials are directed to coding staff, Prior authorization denials directed to Utilization Management for review, others are worked by billing staff
- Monitor
- Track and Trend incoming denials.
- Create a denial log
- Audit & Evaluate Employee production
- Resource availability
- Ensure employees have the necessary tools to be effective
- Prevent
- By Tracking and Trending denials collaborate with team on prevention
- Add edits to clearing house for common denials
Following these steps when setting up or restructuring your denials management process and can ensure a successful revenue cycle.
Avoiding automatic rebilling
Read more : Which Use Of Figurative Language Most Clearly Conveys Playfulness
The “trend” to automatically rebill a claim causes more work and slows productivity of billing staff. If a bill is automatically resubmitted when a denial or rejection is received, additional denials are likely to follow. Resubmitting a denied claim without the proper resubmission indicators can cause another denial for duplication.
Duplicate denials are quite common when automatically rebilling claims. If denials or rejections are received, it is imperative to have a staff member review and investigate the reason and respond accordingly. Once the denial is reviewed and changes are made a “corrected claim” can be submitted with appropriate indicators.
Coding to the most specific level
Coding to the most specific level is critical as using nonspecific codes can cause underpayments, rejections or even denials. To avoid any payment delays, ensure coding to the highest specificity for coding completeness. If necessary, use placeholders such as X to obtain the seventh character.
Pro Tip: If necessary, use placeholders such as X to obtain the seventh character.
Step 3: Monitor
Why is it important to track and trend denials and rejections of claims?
Preventing denials is always one of the top priorities of any healthcare provider. Unfortunately, not all denials can be prevented. Tracking the trend of denials and rejections is a helpful tool in prevention as well. Tracking denials and rejections can provide insight into understanding the cause of the denial. Once the problem is identified, the proper correction can be determined.
Tracking denials encourages ongoing improvement in the revenue cycle. If there are an abundance of prior authorization denials, check with the Utilization Management department to determine if the denials are due to late submission or medical necessity.
Many denials are due to missing information in patient demographics, coordination of benefits or eligibility issues. Once common denials are identified and tracked, trends and resolutions for future improvement can be determined.
JTS offers nCREAS™ Analytics as a Service, a proprietary, predictive solution for enhancing operational performance including denial management. nCREAS™ enables healthcare organizations insight into the reason for denials and tracks them over time.
Analyze denials and rejections
Claims denial data can be captured by two different methods. Collecting the 837, 835 and 277 file will show the clean claims rate, denials rate and specific denials information that can be reviewed. These files are copied from the facility’s clearinghouse system and are in a standard format across all payors. The denial information can also be captured from the reporting system of the organization’s practice management software. This data is easier to manage since it has been processed. Depending on the robustness of the management software processes data, additional reporting may not be needed. Typically,  facilities would then extract the denials report from the practice management software and load it into a spreadsheet program to do further analysis. Some facilities have an additional reporting program like Power BI or Tableau to download those extracts and start a dashboard. The raw 837, 835 and 277 data will require some type of database reporting system. Even if your practice management software processes the data, the ideal situation would be to have a database reporting system linked to a Power BI or Tableau. Either way, the extracted data will go into an analytics dashboard. These dashboards list key performance indicators (KPIs), show trends over months and years and many other powerful calculations. Having the data available in a consistent format and the ability to go back over the course of time allows benchmarking and determining when metrics are in or out of the established range.
facilities would then extract the denials report from the practice management software and load it into a spreadsheet program to do further analysis. Some facilities have an additional reporting program like Power BI or Tableau to download those extracts and start a dashboard. The raw 837, 835 and 277 data will require some type of database reporting system. Even if your practice management software processes the data, the ideal situation would be to have a database reporting system linked to a Power BI or Tableau. Either way, the extracted data will go into an analytics dashboard. These dashboards list key performance indicators (KPIs), show trends over months and years and many other powerful calculations. Having the data available in a consistent format and the ability to go back over the course of time allows benchmarking and determining when metrics are in or out of the established range.
Step 4: Prevent
How to help prevent medical billing claim denials
The formal definition of a medical billing denial is, “the refusal of an insurance company or carrier to honor a request by an individual or provider to pay for healthcare services obtained from a healthcare professional.” A denial is not a rejection, yet both result in underpayment or no payment. Ensuring effective steps to prevent denials is essential to an effective revenue cycle.
- Create a task force that analyzes denial trends to determine if additional resources are needed. Also, the task force can implement additional tracking and report processing to develop solutions.
- Improve patient access quality measures. Ensure patient registration is effective in obtaining all correct patient information. Ineffective registration can cause many denials and rejections.
- Go beyond generic coding and code to the highest specificity.
- Ensure all revenue cycle representatives have a prevention mindset.
- Optimize claim management software. Confirm all claim edits are up to date to improve the clean claim rate. Maintaining a clean claim rate of 80% or higher ensures rejections and denials are kept at a minimum.
- Work with payors, ensure contacts are current and payments are received at negotiated amount. One big miscommunication within revenue cycle is the addition of more revenue cycle representatives will ensure a reduced denial rate. This is incorrect if the steps of prevention are in place additional representatives are not required.
Ready to transform your organization?
Denial management in healthcare is a key component of the revenue cycle. While denials can greatly impact hospital cash flow, they can also be avoided by having properly educated billers and following the steps listed in this article.
Source: https://t-tees.com
Category: WHICH