
Making an informed decision about permanent birth control, tubal ligation or vasectomy is important.
There are many reasons individuals or partners consider permanent birth control: They’re worried about passing on a genetic disorder to a child, don’t want to have biological children or pregnancy poses a risk.
You are viewing: Which Is More Reversible Vasectomy Vs Tubes Tied
Dr. Nicholas Toepfer, a UCHealth urologist, and Dr. Chelsea Drake, a UCHealth OB/GYN, answer common questions about tubal ligations (tubes tied) and vasectomies to help with decision making.
Jump to information on vasectomies
Women’s permanent birth control options
What is tubal ligation?
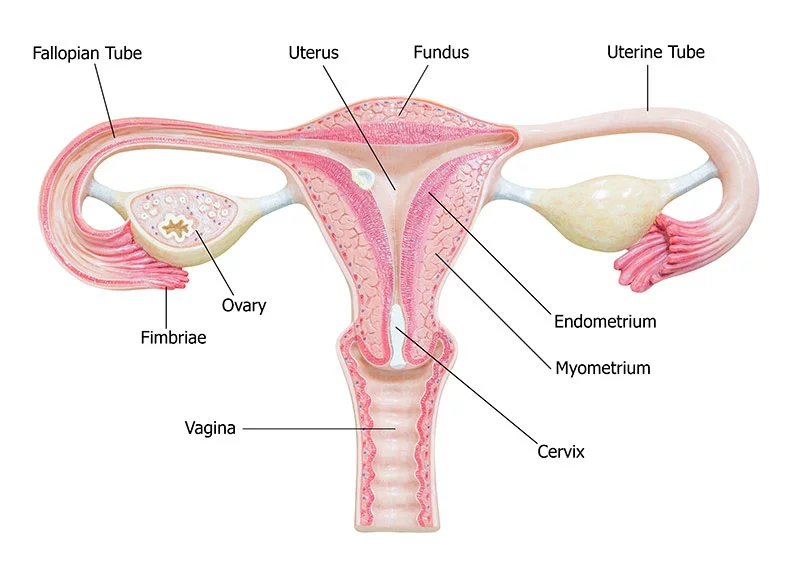
Commonly known as “getting your tubes tied,’’ tubal ligation is a surgical procedure that prevents you from getting pregnant. The “tubal” part refers to the fallopian tubes, and “ligation” means tied off. Fallopian tubes connect the ovaries to the uterus and provide the passageway for unfertilized eggs. By tying a woman’s tubes, the eggs released each cycle cannot meet up with sperm for fertilization.
A tubal ligation doesn’t prevent sexually transmitted diseases.
Why would one want to get a tubal ligation?
Tubal ligation is a permanent birth control method that reduces the chances of getting pregnant to 1%. Unlike birth control pills and other methods, tubal ligation doesn’t affect a woman’s hormones, change periods or bring on menopause. There are no side effects, such as mood swings, weight gain, headaches, or cramping and spotting, that may come with other birth control methods.
Some women may choose to have a tubal ligation because they do not want children. Others may consider the option if pregnancy is a health risk or if one of the partners has a genetic disorder they want to avoid passing on to a child.
Does a tubal ligation lessen my chance of ovarian cancer? When might I want to consider it as preventative cancer care?
“We have learned that most cases of ovarian cancer start in the fimbriated ends (also known as fimbriae tubae), the small fingerlike projections at the end of the Fallopian tubes,” said Dr. Chelsea Drake, an obstetrician and gynecologist with UCHealth Women’s Care Clinic – Windsor.

Removing both Fallopian tubes, called a bilateral salpingectomy, decreases a woman’s future risk of ovarian cancer by about 50%. Partial salpingectomy reduces her risk by about 25%.
Hormonal birth control methods (such as IUDs, injections or pills) also decrease a woman’s risk of uterine, ovarian and colon cancer for all women, not just those with a genetic predisposition, she said.
Some women have genetic mutations that significantly increase their risk of ovarian cancer. Removal of Fallopian tubes (and ovaries) is recommended after a certain age in these women. People can talk to a genetic council to better understand the genetic risks of specific cancers and how to test for those risks.
How is tubal ligation done?
While under general, local or spinal anesthesia (similar to what is used during a cesarean section), an OB/GYN surgeon will block or cut both Fallopian tubes.
“The approach depends on timing and the surgical technique,” Drake said. “Your doctor will go over the details before surgery.”
The surgeon can either remove a piece of each Fallopian tube, called a partial salpingectomy, or completely remove the Fallopian tubes, called a bilateral salpingectomy. Other types use clips or bands applied to block the fallopian tubes or the tubes are burned (cauterized).
“Partial and complete salpingectomies are the most common techniques used these days,” Drake said.
At the time of cesarean delivery, any technique can be used, she said.
Immediately following a vaginal delivery, a small 3- to 4-centimeter incision is made below the belly button. The tubes are visualized through the incision, and a small piece of each tube is removed, or clips or bands are used, Drake said. Cauterization and bilateral salpingectomy are not used in this scenario. This procedure is done under general or spinal anesthesia, and most women go home the next day.
In cases remote from pregnancy, called interval sterilization, the surgeon will make one or more small incisions near the belly button or, in some cases, in the lower abdomen. Using a small laparoscope (camera), they find the Fallopian tubes and either remove, clamp, band or seal off the tubes with an electric current. The incisions are then closed with one to two stitches. Tubal ligation is an outpatient surgical procedure, and most patients can go home the same day.
In all scenarios of tubal ligation, the skin is closed with dissolvable sutures.
Are there qualifications I have to meet, such as being a certain age, to get a tubal ligation?
In general, a woman requesting a tubal ligation must be at least 18 years of age and capable of giving informed consent. There are no fertility or other health prerequisites, Drake said.
Medicaid requires women to be at least 21 years of age. Some insurance providers, including Medicaid, require consent forms to be signed at least 30 days in advance. Those consent forms are the same as for any surgical procedure and do not require spousal/significant other approval or co-signature, Drake said.
“As women’s health care providers, we strive to educate patients and engage in shared decision-making,” Drake said. “It is important to consider the potential risks and benefits of permanent sterilization compared to reversible forms of contraception. We don’t want anyone rushing into a permanent decision like this. The risk of regret is about 20% in women under age 30, compared to about 5% in women over 30.”
Will insurance pay for a tubal ligation?
Most insurance companies consider this elective surgery and will cover at least a portion of the cost. Co-pays do exist, depending on your insurance provider and specific plan.
What is the recovery time?
Recovery times for tubal ligations are different based on the scenario:
- Recovery is six weeks if performed at the time of a C-section, the same as if a C-section was performed without tubal ligation.
- Recovery is two weeks if performed laparoscopic outside of pregnancy or immediately following vaginal delivery.
Patients should not lift heavy objects during the recovery period or engage in strenuous activities such as exercise. They can perform most normal day-to-day activities.
What are the side effects of tubal ligation? Will there be scars?
Tubal ligation does not affect hormones or periods, so there are no long-term side effects if the surgery is uncomplicated. There will be small scars on your abdomen, Drake said.
What is post ablation tubal sterilization syndrome, and should I be worried about it?
Post ablation tubal sterilization syndrome (PATSS) is a condition that can occur in women who have had both an endometrial ablation and tubal ligation.
Read more : Which Of The Following Is True Of Phishing
“Endometrial ablation is a surgical procedure to treat heavy menstrual bleeding but does not prevent pregnancy,” Drake said. “Women who have had this procedure must continue using effective contraception as pregnancy becomes a high risk.”
PATSS is characterized by cyclic pelvic pain due to menstrual blood trapped inside the uterus or fallopian tubes due to scar tissue. In some cases, pain is alleviated by completely removing the fallopian tubes or using hormones to suppress menstruation. Other times a hysterectomy is necessary.
Can doctors perform a tubal ligation after my vaginal delivery or C-section? What are the benefits of doing it during that time?
Tubal ligation can be performed at the same time as cesarean delivery. You and your doctor will discuss the specific technique. Benefits include avoiding a second surgical procedure. It does not change the type of anesthesia used for cesarean delivery. The doctor would still use a spinal or epidural unless general anesthesia is needed.
Tubal ligation also can be performed within a few days of vaginal delivery before being discharged from the hospital, also under spinal or general anesthesia. In this case, you don’t have to return to the hospital another time.
Can tubal ligation be reversed?
Tubal ligation is not recommended if a patient has any doubts they may want to have biological children in the future, Drake said.
Another surgery can reverse tubal ligation, called tubal reanastomosis or tubal anastomosis, but only about 50-80% of women can become pregnant after having their Fallopian tubes reattached.
“Live birth rates after tubal reanastomosis are about 50%, similar to success rates with IVF,” Drake said. “The risk of ectopic pregnancy is 2 to 3%. It also is difficult to find a surgeon who is experienced in performing this procedure.”
An ectopic pregnancy is where a fertilized egg attaches outside the uterus. It can be life-threatening if untreated.
Can I get pregnant after having a tubal ligation? And if so, is there an increased risk for complications or miscarriage?
Drake breaks down the failure rates (the chance of getting pregnant after using specific birth control methods):
“Failure rates for tubal ligation are about 1% but vary depending on the technique,” Drake said.
- Partial salpingectomy has a failure rate of about 1% over 10 years.
- Burning the tubes and using a clip or band have failure rates of 2 to 3% over 10 years.
- Pregnancy is exceedingly rare with the complete removal of both Fallopian tubes. There are case reports in the literature, but it is so rare it’s difficult to assign a percentage.
Contraceptive implant failure rates:
- Nexplanon failure rate 0.05%
- Copper IUD failure rate 1.5%
- Progesterone IUD failure rate 0.5 to 1%
Will I continue to have my period or undergo menopause after a tubal ligation? Does it help with those side effects, such as cramping?
A tubal ligation does not affect hormones, periods, the timing of menopause or menstrual symptoms.
Does tubal ligation lead to early menopause?
No, tubal ligation doesn’t affect the timing of menopause.
Does a tubal ligation affect sex?
No, a tubal ligation doesn’t physically affect sex, nor does it affect one’s hormones.
Can cut Fallopian tubes grow again?
After partial salpingectomy, the cut ends of the Fallopian tubes can heal back together and lead to pregnancy or ectopic pregnancy. As mentioned before, the failure risk of a partial salpingectomy is about 1%.
If the Fallopian tubes are completely removed, they do not grow back.
With tubal ligation, are there increased or decreased risks for other issues, such as ovarian cancer?
Because we now know that most cases of ovarian cancer start in the fimbriated ends of the fallopian tubes, a bilateral salpingectomy decreases a woman’s future risk of ovarian cancer by about 50%, Drake said. A partial salpingectomy reduces her risk by about 25%.
How is a tubal ligation different than a hysterectomy?
Tubal ligation is a minor surgical procedure compared to hysterectomy, with a shorter operating time, lower risk of complications, and quicker recovery period.
Complete hysterectomy refers to the removal of the uterus and cervix. Partial hysterectomy means the cervix is left behind (rarely done, usually only in particular circumstances). The Fallopian tubes are generally removed at the time of hysterectomy. The ovaries can be removed or left behind depending on a woman’s age and situation.
Can I get a hysterectomy to prevent me from having children?
“Hysterectomy is never done solely for contraception,” Drake said.
A hysterectomy is a major operation and is recommended as a treatment option for certain diseases only when other options have been unsuccessful. While a hysterectomy does result in sterilization, it is not performed for this reason alone.
When and why does a woman get a hysterectomy?
Again, a hysterectomy is only used when other treatment options have not worked. It is a major surgical procedure to remove the uterus and has a longer recovery time than less invasive treatments.
Health problems that affect the female reproductive system, such as heavy periods, long-term pelvic pain, non-cancerous tumors (fibroids) and cancers of the ovaries, uterus, cervix or fallopian tubes, may require a hysterectomy.
Hysterectomy may be performed for gynecologic cancers, for genetic mutations that place a woman at high risk for uterine cancer, in women with heavy periods or pelvic pain after medical therapy has failed, or in women undergoing surgical repair of pelvic organ prolapse.
Vasectomy: men’s permanent birth control option
What are a male’s permanent birth control options?
A vasectomy is one of the most effective birth control options for men, but it is “permanent.” The outpatient procedure done under local anesthesia is performed by a surgeon and is where they cut and seal the tubes that carry sperm.
How is a vasectomy performed?
There are two types of methods used to perform a vasectomy, but the ‘no-scalpel technique’ is the only one used at UCHealth.

“The “no-scalpel technique” is the gold standard procedure now,” said Dr. Nicholas Toepfer, a urologist at UCHealth Urology Clinic – Colorado Springs. “This is done through a small opening, resulting in less pain, fewer complications and faster recovery.”
Read more : Which Toyota Rav4 To Avoid
He said his patients meet with him before the 20-minute procedure to discuss details. If his patients feel they need an anti-anxiety medication, one is given by mouth one hour before the appointment.
The technique for the procedure varies by the surgeon, Toepfer said. He said he cuts a 1-centimeter segment of the vas deferens, the long tube that transports mature sperm to the urethra in preparation for ejaculation. He then cauterizes the inner channel of the tube on each end to cause the channel to scar down and become obstructed, after which he ties off each end with an absorbable suture that dissolves over a few months.
“This has to be done on both sides,” he said. “These three techniques reassure us that a failure is very unlikely.
“The opening used during the procedure is so small that in most cases, a stitch is not necessary to close the incision, and you can barely see the opening after one week,” Toepfer said. “I do not use metal clips that some doctors use, so patients do not have to worry about having metal in their bodies after the procedure.”
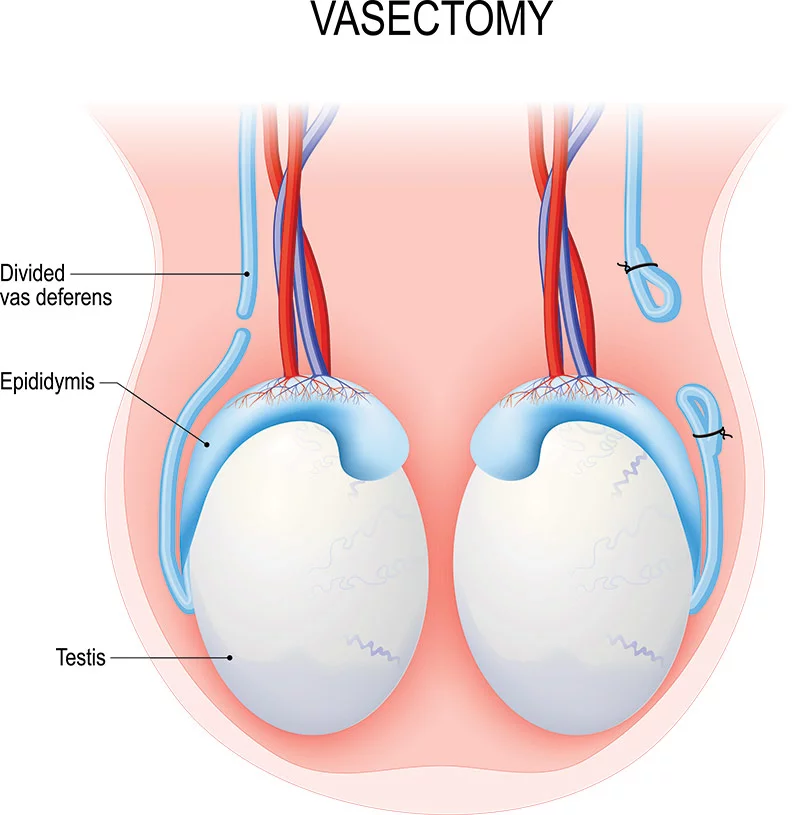
A vasectomy results in the sperm not being able to travel up the vas deferens, and therefore, the man’s semen does not have sperm in it.
“It is important to know that men aren’t sterile until three months after the procedure,” Toepfer said. “That is when a semen analysis is performed confirming that other forms of birth control are no longer necessary.”
Why might a couple choose one option of permanent birth control (vasectomy vs. tubal ligation) over another?
“Vasectomy has the lowest risk of failure (unwanted pregnancy) among all sterilization or birth control options, including tubal ligation,” Toepfer said.
Vasectomy failures occur in only 0.03-0.05% of men who have a vasectomy.
Does insurance pay for a vasectomy?
Most insurance companies will cover the cost of a vasectomy that is done in an outpatient setting. You should always check with your insurance provider before undergoing an elective procedure to understand your out-of-pocket costs, including co-pays, deductibles or out-of-network provider fees.
If you don’t have insurance, check with the health care provider to see what options you might have within the community.
“Many men choose to have their vasectomy in the same calendar year as the birth of their youngest child, so they have already met their family deductible,” Toepfer said.
Is a vasectomy operation painful?
The procedure is performed using local anesthesia, so patients feel very little during the process.
In most cases, your doctor will recommend you take it easy for a few days, using over-the-counter ibuprofen, ice and tight-fitting underwear.
“Most men report the discomfort after the procedure as very mild and don’t need or want to take prescription medication,” he said.
How long does the discomfort after a vasectomy last? And what is the total recovery time?
There is no limitation to walking or leaving the house. In most cases, patients can resume “normal daily activity” on the same day as the procedure.
Men should refrain from sexual activity, exercising or heavy lifting (greater than 15 pounds) for seven days after a vasectomy.
“For most men who have the procedure on a Friday, they are back to work on Monday. And men who work from home find they need little or no time off from work,” Toepfer said. “Men who have jobs requiring strenuous activity or heavy living will need to be limited to light duty for one week.”
Does a vasectomy affect sex?
A vasectomy has no impact on erectile function, libido or sexual functions and sensations. It does not change testosterone values. Men will still ejaculate when they orgasm, but there will be no sperm in the semen.
Does a vasectomy lead to testicle atrophy over time, or does it increase one’s risk of prostate cancer?
A vasectomy does not lead to atrophy over time or cause the testicles to feel different. The testicle will continue to make normal amounts of testosterone and sperm, and the sperm will reabsorb once it has lived its expected lifespan.
Studies have proven that there is no increased risk of prostate cancer or other diseases in men who have had a vasectomy, Toepfer said.
Are there requirements, such as age or having had children, to be able to get a vasectomy?
There is no age requirement to have a vasectomy (besides being 18), and you do not have to be married or have had children.
“Because the procedure is intended to be permanent, we ask men to go into the procedure close to 100% certain that they do not want more biological children,” Toepfer said.
Can a vasectomy be reversed?
“Yes,” Toepfer said. “But we do not support men having a vasectomy if they think it is likely they will want a reversal in the future.”
Vasectomy reversals are often not covered by insurance. It can become an expensive out-of-pocket cost because it’s done in an operating room under general anesthesia.
People’s circumstances and minds do change, so if someone wants to have children after a vasectomy, there are options,” he said. “But if someone is not sure they are finished having children, non-permanent birth-control options are probably best.”
Are there any other permanent birth control options out there?
“Not for men,” Toepfer said. “Tubal ligation and other procedures for women are options, but they usually have a higher risk of complications and may cost more.”
Return to information on tubal ligation
Source: https://t-tees.com
Category: WHICH
